 Acne Scar Treatment: Dermabrasion
Acne Scar Treatment: DermabrasionEverything You Need To Know About Fungal Acne
Anyone who has experienced acne knows that not all pimples are created equal. If your usual breakout-busting treatments aren’t working, you may be dealing with fungal acne.
Acne is considered the most common skin condition in the United States. The American Academy of Dermatology (AAD) reports that some 50 million Americans from adolescence through adulthood deal with breakouts every year. Anyone who has experienced acne knows that not all pimples are created equal, and it can be difficult to know exactly what subtype of the condition you are dealing with. For instance, is your acne bacterial or fungal in nature? Since treatment protocols differ by type, we’re breaking down everything you need to know about the difference between the two.
What Is Fungal Acne?
More often than not, conversations about acne are focused on acne vulgaris, which involves the blockage and/or inflammation of the hair follicles and sebaceous glands. “Traditional acne is often associated with cutibacterium acnes and is often related to other factors as well including increased oil production, clogged pores, and inflammation,” explains Marisa Garshick, MD, a board certified dermatologist in New York City. “In some cases, it can also result from hormonal changes.”
But not all acne patients are diagnosed with acne vulgaris. Fungal acne is another subtype. Also known as pityrosporum folliculitis or malassezia folliculitis, fungal acne specifically impacts the hair follicle. “Pityrosporum folliculitis is due to the overgrowth of a normal yeast that lives on the skin, known as malassezia, that can lead to inflammation of the hair follicle,” Dr. Garshick says.
It should be noted that the yeast responsible for fungal acne is always present on your skin, says Snehal Amin, MD, a board certified dermatologist in NYC. Under normal circumstances, the body is usually able to balance the yeast, but overgrowth can occur leading to the acne-like symptoms. “These breakouts are often triggered by low immunity, high sugar levels, or recent antibiotic treatment,” he explains. “Long-term steroid use can also cause fungal acne.” Warm, humid environments and trapped moisture can both disrupt the balance of bacteria and fungi on the skin.
How to Diagnose Fungal Acne
Acne vulgaris presents as non-inflammatory lesions (comedonal whiteheads and blackheads), inflammatory lesions (papules, pustules, cysts, and nodules), or a mixture of both. In the majority of cases, it is most commonly found on the face, back, and chest. While it’s easy to confuse the two, there are some key differences to keep an eye out for when it comes to identifying fungal acne:
- Type of Breakout: Fungal acne is generally characterized by small, pus-filled whiteheads or pimples that present in clusters on the skin.
- Size of Bumps: Unlike bacterial breakouts, the bumps tend to be similarly sized.
- Areas Affected: Fungal acne is most commonly found on the back, arms, and chest, though it may also present on the face.
- How It Feels: While bacterial acne can be painful, fungal acne is often itchy.
Dermatologists diagnose fungal acne by studying the area(s) of concern. “While the diagnosis may be made clinically during a routine dermatology examination, sometimes a scraping, biopsy, or culture may be taken to confirm the diagnosis,” Dr. Garshick says. Fungal acne does not usually respond to traditional acne treatments, so sharing a list of products or remedies you have previously tried to treat the bumps with may help your doctor hone in on the cause.
How to Treat Fungal Acne
While your typical acne-fighting arsenal may not be as effective in clearing up fungal breakouts, there are still a wide-range of at-home and in-office solutions available. Below, Dr. Amin and Dr. Garshick share their go-to fungal acne treatments — and even how to deal with a last-minute pimple emergency!
1. Topical Skincare
In place of the retinoids, salicylic acid, and benzoyl peroxide used to treat bacterial breakouts, skincare routines for fungal acne usually involve antifungal ingredients such as ketoconazole or selenium sulfide. Creams, gels, and even medicated shampoos featuring the actives can all have a clarifying effect, Dr. Garshick notes.
From there, Dr. Amin says it’s best to keep the rest of your topical regimen simple until the breakout clears. “An inexpensive moisturizer made specifically for the face, such as CeraVe or Neutrogena, is good to help the skin heal,” he says. “During an outbreak, it is best to avoid unnecessary sunscreens, makeup, and so forth.”
2. Oral Medication
In cases where topical treatments aren’t enough, oral antifungal medication may be necessary. These medications work by either preventing the fungus cells from growing or by killing the fungus that is already present. Your dermatologist will be able to prescribe these treatments as needed, in addition to developing a more holistic plan to prevent future fungal breakouts.
3. Cortisone Injections
“There is no overnight cure for acne,” Dr. Amin laments. But that’s not to say your dermatologist can’t help you out in a pinch. If a pimple pops up at the last minute before a big event, he says to reach out to your provider. “Sometimes, just reducing the inflammation around a pimple restores the bacterial and fungal balance,” Dr. Amin explains. “That’s what a cortisone shot from your dermatologist can do without antibiotics or antifungals.”
Patient Perspective
No matter what type of acne you have, the trial and error of the treatment process can be trying. Sascha is a patient who experienced fungal acne for years before finally finding a solution that worked for them with the help of a dermatologist. Here, they share their experience of getting the correct diagnosis and working out a skincare routine that was able to clear up their breakouts.
The AEDITION: How did you receive your fungal acne diagnosis?
Sascha: I first noticed bumps on my shoulders and back and didn’t pay much attention to them because they weren’t too expansive. Over time, the patches became more problematic, and I started trying out various treatments myself — mostly toners and lotions — but nothing ever worked very well. I became more self-conscious as the areas got more prominent. I wanted to get to the bottom of the problem, so I went to a dermatologist. It was my first time going to a dermatologist! As soon as I went over the list of products I’d tried that didn’t work, she said she had an idea of what it was. That was confirmed once she took a look at it. I spent a while wishing I’d gone to a doctor sooner, but I’m so happy I got around to it eventually.
The AEDITION: What treatments ended up working for you?
Sascha: We tried out some topical antifungals to start with, which helped but didn’t clear the problem completely. I was also advised to use a specialist shampoo because I was experiencing an itchy scalp and had patches on my upper neck. My dermatologist then prescribed an antifungal medication that I took for a short while, and that’s what finally started working. I had some scarring because the breakouts had been there for so long, so I used a gel that my dermatologist prescribed and it’s cleared up well now.
The AEDITION: Do you have any advice for other people dealing with acne?
Sascha: My number one piece of advice — understandably, given my experience with it — would be to go to a dermatologist. Although the breakouts I had weren’t super visible, they affected my self-confidence very negatively, and trying all these supposed solutions but not getting any results was so demoralizing. There’s absolutely a psychological aspect to recovering from acne and regaining self-confidence takes time. In the same token, though, I don’t think people should feel the need to hide away simply because of clogged pores. That’s all it is. There shouldn’t be as much stigma about it, and that’s the message that I think is important to share.
The Takeaway
Fungal acne may bear some similarities to acne vulgaris, but the cause of the two skin conditions is very different. As such, traditional acne treatments (like over-the-counter skincare) will likely not be effective. Consulting with a board certified dermatologist is the best way to diagnose fungal acne, and they will be able to develop a treatment plan that will have you back on your way to clearer skin.
All products featured are independently selected by our editors, however, AEDIT may receive a commission on items purchased through our links.
More Related Articles
Related Procedures
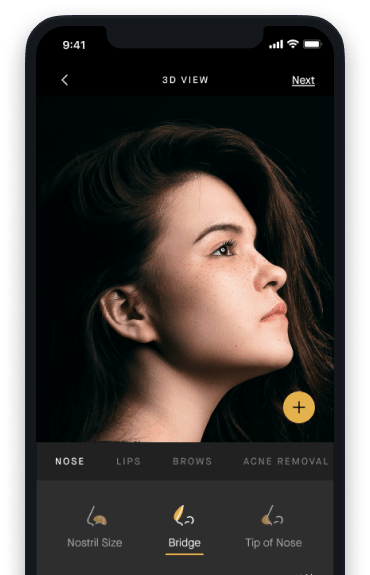
AI Plastic Surgeon™
powered by'Try on' aesthetic procedures and instantly visualize possible results with The AI Plastic Surgeon, our patented 3D aesthetic simulator.
