Breast Augmentation with Implants
Breast Augmentation with ImplantsA Comprehensive Guide To Breast And Nipple Reconstruction
From immediate and delayed implant reconstruction to the numerous types of flap surgeries, The AEDITION has compiled an in-depth guide to post-mastectomy breast and nipple reconstruction.
*Since 1985, October has served as Breast Cancer Awareness (BCA) Month — a period devoted to educating the public on the disease that, according to the Centers for Disease Control and Prevention (CDC), is the second most common form of cancer in women, regardless of race or ethnicity. Men can also be diagnosed with breast cancer (albeit at a much lower rate), and The AEDITION is devoting much of its coverage this month to BCA, from expert guides to mastectomies and reconstructive breast surgery to powerful patient perspectives and roundups of products that give back. *
Now that you have a better understanding of the physical and emotional toll of breast reconstruction and the importance of finding the right surgical team (read our overview of how to approach the breast and nipple reconstruction process HERE), it is time to dive deeper into the surgical options that exist for post-mastectomy patients to reconstruct their breasts and nipples.
Generally speaking, there are two categories of breast reconstruction: implant-based and autologous tissue (a.k.a. “flap”) based. In some cases, a combination is used to achieve the most natural and symmetrical results. Similarly, there are two main types of nipple reconstruction. One involves tattooing alone, while the other is a hybrid of reconstruction and tattooing.
“I want all of my patients to understand their options so that they can make the best choice for them,” says Nashville-based board certified plastic surgeon Jacob Unger, MD, who performs hundreds of breast reconstructions a year. “And then my job is to give the best result I can under those constraints.”
Here, a comprehensive guide to the most common types of breast and nipple reconstruction.
Reconstruction With Breast Implants
The most popular form of breast reconstruction, breast implants offer a shorter surgery and recovery time than other reconstructive procedures. Implant reconstruction can either be delayed (performed in the months following mastectomy) or direct (performed in conjunction with the mastectomy surgery), and medical advances — like skin-sparing mastectomies, cohesive gel silicone implants, and internal support technologies like AlloDerm and GalaFLEX mesh — have allowed surgeons to create increasingly natural-looking results.
Despite the popularity, the technique is not without fault. “The challenge with implant-based reconstruction is that there is no natural soft tissue of the breast to help camouflage and contour an implant or to help rearrange tissue and nipple position in the same way that you can when there’s native breast tissue,” says Dr. Unger.
With that in mind, it is important to understand the different facets of implant-based reconstruction.
Pre-Pectoral Implant Placement
While breast implants (both reconstructive and cosmetic) have historically been placed under the pectoral muscle to help achieve a more natural look, the trend is now toward pre-pectoral (read: over-the-muscle) placement.
“Pre-pectoral implants allow for an easier recovery with less pain and discomfort,” says UCLA board certified plastic surgeon Jason Roostaeian, MD. Another perk? The lack of animation deformity. “When you have an implant under the pec muscle and you flex it, and it makes things look a little off,” he shares.
<captionimg url={https://images.ctfassets.net/zw35sfestf1t/4kgymfwgzdvico4ryaozgb/7b738a9b9c468daccac9743810d02f07/jacobunger__1_.jpg}>
A before-and-after of Dr. Unger's pre-pectoral breast reconstruction following a nipple-sparing mastectomy.
Ideal candidates for pre-pectoral placement are those with younger, thicker skin, which better camouflages the implant directly below. Technique is also important. “Wrapping the implant in a dermal matrix (sterilized cadaver skin) allows you to contain the implant well and gives it an extra layer of coverage,” Dr. Roostaeian notes. “But the most important technique we use to disguise the implant is fat grafting.”
Rather than using an implant alone, plastic surgeons will often recommend a hybrid procedure that involves harvesting fat from a donor site (think: the belly, flanks, or inner thighs) to be injected around the breast implant. The result? Smoother and more natural-looking breasts.
“Fat grafting has changed the way I do breast reconstruction,” says Beverly Hills-based board certified plastic surgeon Leif Rogers, MD. “It can improve the outcome of any breast reconstruction, creating a more natural appearance and giving me the ability to fine-tune my results in a way not previously possible.”
Additionally, Dr. Rogers has been having success with a new liposuction-alternative called Renuva. “Renuva is a biological allograft product that stimulates your body to grow its own fat cells,” he says. “This would be an ideal product for small contour irregularities after breast reconstruction as opposed to using a patient’s own fat.”
Delayed Reconstruction Using Implants
Depending upon a patient’s individual anatomy and treatment plan, he or she may choose not to combine their mastectomy and reconstruction procedures. Similarly, surgeons may recommend delaying the placement of permanent breast implants until a later date for better results.
In such cases, tissue expanders are sutured into the breast pocket immediately following the mastectomy. In the weeks and months following the surgery, the expanders are gradually inflated in a plastic surgeon’s office using air or saline. “A tissue expander preserves the space where the breast needs to be,” says Dr. Unger. And, since placing a heavy silicone implant into an empty breast pocket would compress the fragile blood supply that remains post-mastectomy and lead to tissue death, he notes that the tissue expander “allows the mastectomy flaps to rest without putting undue weight there.”
<captionimg url={https://images.ctfassets.net/zw35sfestf1t/qwzb5aiwpqk0olqhtinqd/617149c0afa434bc6b455775044c2c95/dr_jason_plastic_surgery_breast_reconstruction_subpec_implant_f__2_.jpg}>
A before-and-after of Dr. Roostaeian's unilateral subpectoral breast and nipple reconstruction.
Although the expansion process can be uncomfortable, tissue expanders have the additional benefit of giving both plastic surgeons and their patients time to home in on an aesthetic goal. Once the expanders reach the appropriate size, they are exchanged for permanent breast implants. Dr. Roostaeian’s patient Caroline* (diagnosed at 39) admits that the expanders proved to be a necessary evil. “My expanders didn’t look natural, and were sometimes very painful after they were filled,” she recalls. “But they helped me get a really good idea of what size implants would ultimately be best for me.”
After years of monitoring benign tumors and then a cancer diagnosis at age 31, Dr. Unger’s patient Laura says she chose a nipple-sparing double mastectomy because of the quality of reconstruction available today. “I was tired of the breasts I had, but I wasn’t ready to give them up completely,” she confides. “I was really lucky because he was able to place the expanders on top of the muscle, which was a lot easier recovery for me.”
Laura chronicled her journey on Instagram @laura_birdwell and her blog, tatatocancer, and, once her expanders were filled, Dr. Unger exchanged them for permanent implants and performed simultaneous fat grafting. Like many reconstruction patients, Laura then had an additional surgery to further refine her results. “I think they look better now than they did before,” she says of her breasts.
Direct-to-Implant Reconstruction
In some cases, women can skip the expander step by having their permanent breast implants placed immediately after their mastectomy. With its promise of only one surgery (which means less anesthesia and recovery time), the direct-to-implant option is understandably appealing — though it’s not for everyone.
According to Dr. Unger, good candidates are usually women with “smaller, ideally shaped breasts,” who “want to be close to the same size, are very healthy, and have very robust mastectomy flaps” (read: ample blood supply).
Hayley, diagnosed at age 30, initially had a lumpectomy. “That gave me time,” she says of the procedure. “They got the tumor out, and found out it hadn’t spread.” In her search for a highly skilled surgeon with experience performing pre-pectoral, direct-to-implant reconstruction, Hayley found Dr. Roostaeian after interviewing five or six surgical teams.
During this kind of reconstruction, Dr. Roostaeian uses a new fluorescence imaging technology called SPY to evaluate blood flow right in the OR. “It’s another tool in our arsenal to help ensure the long-term success of the reconstruction,” he says.
Kelly, diagnosed at 45, opted for a unilateral mastectomy and immediate reconstruction with Dr. Rogers. “I had cosmetic implants, and I really liked how I looked before,” she shares. “Whether or not to have reconstruction was never a question in my mind.”
She was able to undergo a sub-pectoral, direct-to-implant reconstruction, in part because she already had breast implants placed under the muscle. Dr. Rogers also replaced the implant in the non-cancer breast to ensure symmetry, and Kelly ended up having a couple of subsequent surgeries — including fat grafting and nipple reconstruction — for further refinement. Eight years later, she is still very happy with the results. “You can’t even tell the difference,” she says.
While there are plenty of direct to implant success stories, there is also risk. Because of the fragile nature of post-mastectomy skin flaps, many surgeons prefer the two-stage (expander followed by implant) process. “Everybody wants less surgery. Everybody wants to be done and have it behind them,” says Michael Newman, MD, a board certified plastic surgeon at South Bay Plastic Surgeons in Torrance, CA. “But it’s more important for me to give them a more durable, long-term result.” He prefers using a tissue expander because “it’s very light” and “doesn’t put any pressure on the skin or the mesh,” which “allows the sutures to heal.”
Additionally, the procedure is seldom as ‘one and done’ as it sounds. Patients almost always require additional surgeries to achieve their aesthetic goals. “Direct to implant is a nice concept,” says Dr. Unger, “But the vast majority of the time, you’re going to need to go back to the operating room to touch things up or round things out or add some fat.”
Flap Reconstruction
Autologous tissue reconstruction — more commonly known as “flap surgery” — involves the transfer of tissue from one area of the body (i.e. a donor site) to the chest to create a breast mound. Surgeons can either shift the tissue from one area to another, leaving the primary blood supply of the donor site intact (a.k.a. a pedicle flap), or completely remove the tissue from its original spot and reattach it to the chest in a free flap procedure.
Free flaps require intricate microsurgery, during which plastic surgeons suture blood vessels together under a microscope to re-establish the blood supply between the donor tissue and the chest. It’s meticulous and time-consuming work (bilateral free flap surgeries can take up to 12 hours to complete), and patients are closely monitored in the hospital for up to five days post-op to ensure the flap is viable.
The recovery process can be more complex than implant surgery because patients have multiple surgical sites to contend with (the chest and the donor area), though patients report similar pain and discomfort levels with each type of procedure.
Types of Flap Reconstruction
Because of the donor site component, there are a variety of flap procedures for a patient to choose from based on their anatomy and aesthetic goals. The names are based upon the donor sites, including those from the abdomen (TRAM and DIEP), back or shoulder (LAT), inner thigh (TUG), and buttocks (GAP).
<captionimg url={https://images.ctfassets.net/zw35sfestf1t/6tvatrx0selcdjyzgiefbf/430d029fe1f2c807e002d916c354e783/10-16-2019_editorial_before-after_breastreconstruction.jpg}>
A before-and-after of Dr. Newman's bilateral DIEP flap breast and nipple reconstruction.
Among the plastic surgeons we interviewed, the most popular flap surgeries are the latissimus dorsi (LAT) flap and the deep inferior epigastric perforator artery (DIEP) flap. While a LAT flap is often used in conjunction with a breast implant reconstruction for better results, the DIEP is a free flap procedure that removes abdominal skin and fat only (similar to a tummy tuck) to create a breast mound.
LAT Flap
- Donor Site: Composed of muscle, skin, and fat from the back
- Type of Flap: A pedicle flap (it remains attached to its primary blood supply)
- Scarring: Creates a donor site scar along the back that can usually be concealed in the bra line and an oblong scar around the new breast mound
- Surgery Time: 5 to 7 hours, on average
DIEP Flap
- Donor Site: Composed of skin and fat (no muscle) from the abdomen
- Type of Flap: A free flap (it is completely detached from its original blood supply)
- Scarring: Creates a donor site scar between the hip bones (similar to a cosmetic tummy tuck) and an oblong scar around the new breast mound
- Surgery Time: 8 to 12 hours, on average
Advantages of Flap Reconstruction
While flap procedures are more complicated to perform and require longer surgery times, Dr. Roostaeian says they remain the “gold standard” for breast reconstruction because they create a result that most closely resembles and behaves like a natural breast.
Unlike an implant, the new breast mound feels more like a natural breast because it is created with the patient’s own fat and skin. In the case of unilateral reconstruction, the plastic surgeon will be better able to match the new breast to the unaffected breast. Additionally, breasts created from flap procedures can fluctuate in size and shape as a patient gains or loses weight.
“Flap surgery is ideal for patients who’ve opted for unilateral reconstruction because that flap changes with your body,” says Dr. Roostaeian, who adds that the results are, long term, much more permanent than implants. “When you choose the implant route, you’re basically signing up for more surgeries in your life because implants tend to have some issues down the road.”
<captionimg url={https://images.ctfassets.net/zw35sfestf1t/35yvu4q4y1iyjmidjqduhu/9a54e787069024a30d7755bb2ce90c84/flap_reconstruction__1_.jpg}>
A before-and-after of Dr. Rogers' unilateral flap breast and nipple reconstruction.
That lack of future revisions led Marjan, one of Dr. Roostaeian’s DIEP flap patients who was 47 at the time of her surgery, to choose the procedure. “I told him that because I was young, I didn’t want to have to go under the knife in my seventies,” she recalls.
Dr. Rogers’ patient Meredith* didn’t want breast implants because she thought they’d look unnatural and possibly interfere with her active lifestyle. “When Dr. Rogers explained that the DIEP procedure would be a tummy tuck — replacing my breasts with my own tissue — and I wouldn't have implants, I was all in,” she shares. “I knew it would be a long 12- to 13-hour surgery the day of, but I was ready to go for it.”
Though she was initially concerned about scarring and the longer recovery time, Meredith is “beyond satisfied” with her reconstruction. And, with her nipple reconstruction also complete, she says her breasts appear so natural that it looks like she had a breast lift and abdominoplasty (i.e. tummy tuck) — not a double mastectomy.
Flap surgery is also an option for women whose implant reconstruction failed due to radiation or persistent capsular contracture issues. Dr. Roostaeian’s patient Caroline originally had bilateral, implant-based reconstruction, but radiation damaged her tissue and caused healing problems. “Dr. Roostaeian told me that the only way to permanently address the situation was to have a DIEP flap,” she says. “It was daunting, and I didn’t think I had enough fat, but he was able to create a small breast and augment it with an implant. It’s so natural that I wish I’d had enough fat to do the other side too.”
Nipple Reconstruction
While skin- and nipple-sparing mastectomies have become commonplace, the patient’s diagnosis may not always allow surgeons to keep the nipples intact. This leaves patients with two reconstruction options: tattooing alone or a combination of surgical reconstruction and tattooing.
In the former, a medical tattoo artist matches the new nipple and areola to the existing one (after unilateral mastectomy) or creates two new nipple/areolar complexes based on the patient’s aesthetic preferences (after bilateral mastectomy). Shading and color variations help create the illusion of depth and projection.
Surgical nipple reconstruction, meanwhile, takes about 45 minutes and can be done either in conjunction with a follow-up reconstructive surgery or alone under local anesthesia. Surgeons use skin from the center of the breast to create a nipple, leaving a small horizontal scar. Patients can then have the areola and nipple tattooed for a more natural-looking color and to conceal any visible scarring.
The Takeaway
Just as no two breast cancer diagnoses are the same, the reconstruction process is a deeply personal experience that patients may choose to undergo when it is most comfortable for them. With that said, understanding the options available prior to having a lumpectomy or mastectomy can ensure the patient ends up with the best results for their anatomy and aesthetic goals. Finding the right surgical team and seeking the support of women and men who have been through the experience can help to make sense of the process.
*Patient names have been changed
More Related Articles
Related Procedures
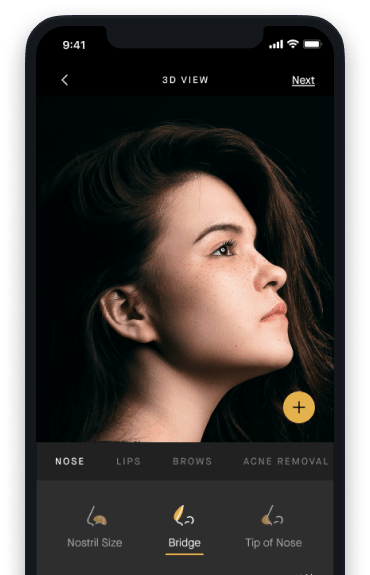
AI Plastic Surgeon™
powered by'Try on' aesthetic procedures and instantly visualize possible results with The AI Plastic Surgeon, our patented 3D aesthetic simulator.