 Upper Eyelid Blepharoplasty
Upper Eyelid BlepharoplastyIs Hypnosis The Future Of Sedation In Plastic Surgery?
Hypnosis has been used to lull people into a semiconscious state for centuries, and it is back in ORs around the globe. So, how and why is this ancient practice making a comeback in modern medicine? The AEDITION asks the experts.
Doctors and patients alike are continually searching for ways to make the surgery experience more comfortable. One of the key components to comfort or the lack thereof is anesthesia (i.e. how — and to what degree — a patient is desensitized and/or sedated during a surgical procedure). Generally speaking, there are four main types anesthesia:
- Local Anesthesia: Desensitizes a small area of the body
- Regional Anesthesia: Numbs a specific part of the body, but a larger one than possible with local anesthetic
- Conscious Sedation: Sometimes referred to as twilight sedation, is used for short procedures or when regional anesthetic would not be effective
- General Anesthesia: Patient is unconscious
Each of these options comes with a particular set of characteristics, risks, and applications and are widely used in medical and aesthetic surgeries and procedures. There is, however, a fifth technique that has been gaining popularity in recent decades — though there is nothing new about it. Hypnosis has been used to lull people into a semiconscious state for centuries, and it is now making its way into operating rooms around the globe. So, how and why is this ancient practice making a comeback in modern medicine? The AEDITION asked the experts.
The History of Hypnosis
There is evidence of hypnosis being used as a healing aid by early Hindus, who took their sick to the temple to meditate overnight. Published in 1027, a Persian text called The Book of Healing was the first to distinguish between sleep and hypnosis. In subsequent centuries, physicians and scientists studied and honed their ‘healing’ techniques, sometimes using religious relics or magnets to ‘cure’ patients.
In the eighteenth century, German doctor and amateur astronomer Franz Mesmer developed his theory of animal magnetism, which hypothesized that all living things possess an energy that could be harnessed by a practitioner for healing. Though his ideas were dismissed as imagination rather than science, Mesmer’s followers continued his legacy and the term ‘mesmerize’ remains.
A century later, Scottish surgeon James Braid sought to debunk the work of Mesmer’s successors by exposing the fraud in their traveling demonstrations. But Braid couldn’t get past one irrefutable fact: None of the mesmerized subjects could open their eyes after staring at a bright object for eight to 12 minutes. Intrigued, Braid set about his own experiments to see if he could replicate the experience himself without magnets, operators, or guides. Braid successfully hypnotized himself, giving rise to the modern “pyscho-physiological” (read: mind-body) theory of hypnotism.
In 1829, French surgeon Jules Cloquet performed the first documented use of hypnosis as anesthesia during a mastectomy in Paris. The technique was first used in America during dental surgery in Boston by dentist Dr. Harwood in 1836, and, three decades later, by field surgeons during the Civil War. Despite the successful cases, the discovery of ether as anesthesia in the mid-19th century proved to be a game-changer for sedation. Compared to hypnosedation, the drug was quicker and more reliable, as not every patient can be successfully hypnotized.
Hypnosis Makes a Comeback
While pre-op hypnotherapy fell out of favor, it never went away completely. In 1992, anesthesiologist Marie Elisabeth Faymonville and colleagues at Belgium’s University of Liege began experimenting with a combination of local anesthesia, conscious IV sedation, and hypnotherapy during breast cancer treatment and other surgeries. To date, the team has performed over 9,000 operations under hypnosis and completed several clinical studies. Results show a significant reduction in both perioperative pain and anxiety, decreased reliance on post-operative medication, and a quicker recovery time from anesthesia.
Breast surgery has a high incidence of chronic post-operative pain — pain that lingers for months, or even years, after a procedure. The degree of perioperative pain (i.e. how much pain a patient experiences immediately after surgery) is also a risk factor for chronic pain. In other words, patients who feel less pain surrounding their procedure tend to have less pain long-term.
One European clinical trial followed two groups of similar breast cancer patients: one who received general anesthesia and one who received local anesthesia and intravenous sedation with hypnosis. Immediately after the procedure, those who had the local anesthesia/hypnosedation combination experienced significantly lower pain and anxiety levels. In the four years that followed (the duration of the study), they saw decreased levels of chronic pain and better range of motion. Researchers admit that more data is needed, but the idea is worth exploring further.
Hypnosedation in the United States
At the MD Anderson Cancer Center at the University of Texas, doctors are conducting clinical trials using similar techniques — combining local anesthesia, conscious sedation, and hypnosis. Initially, the researchers had to overcome some cultural preconceptions surrounding hypnosis. While many people are under the cartoon-inspired assumption that hypnosis will have them clucking like a chicken, it actually allows people to dissociate with reality and enter a deeply relaxed state.
One study focuses on women undergoing breast biopsies and lumpectomies (i.e. the removal of tumors and a margin of surrounding breast tissue). The surgical team includes a breast surgeon, a mind-body specialist, and an anesthesiologist standing by to administer general anesthesia if necessary. Patients are asked to focus on a place of deep relaxation and comfort. They remain conscious, but in a dissociated state — like driving on autopilot — and avoid some of the side effects of general anesthesia (think: grogginess, nausea, and vomiting). In some instances, patients participating in the trial exhibited a decreased dependence on opioids, both during and after surgery.
Hypnosedation for Plastic Surgery
While hypnosis for plastic surgery is uncommon in the U.S., providers are open to the idea. “This will work really well on certain people, as long as you pre-screen patients to make sure they’re amenable to being hypnotized,” says Jason Roostaeian, MD, a board certified plastic surgeon at UCLA.
He’s quick to point out, however, that general anesthesia does not deserve the bad rap it often receives. In most cases, it’s used in combination with local anesthetic to keep doses lower, and, in his opinion, sedation is actually the riskier option. “With general, we can control your breathing because there’s a tube down your throat to keep you alive,” Dr. Jason explains. “But with sedation, there’s a fine line between relaxing someone for surgery and creating a situation where there’s breathing issues.”
Nashville-based board certified plastic surgeon Jacob Unger, MD, agrees that unconscious sedation serves a purpose. “During particularly long procedures or procedures where the airway can be compromised, general anesthesia is the safest option,” he says. “The surgeon and whole surgical team have better control of the patient's hemodynamics and airway.”
When Hypnosedation Is Appropriate
In healthy patients who are appropriate candidates, both surgeons see the potential for hypnosedation in plastic and reconstructive surgery procedures. “Smaller or regional procedures that can safely be performed without medical airway control can be done under local combined with relaxation techniques,” Dr. Unger says, adding that the technique “can aid in rapid recovery.”
Dr. Jason says he would consider using hypnosis during breast augmentation, facelifts, upper blepharoplasty, and even for more invasive and stimulating procedures like liposuction and abdominoplasty. He’s generally open to working with patients who — for medical necessity or personal preference — want to avoid general anesthesia. “I have the same conversation with each of them,” he shares. “I make sure they know that sedation makes me inherently less efficient than general because I’m having to focus on the patient moving or being uncomfortable.”
Dr. Unger agrees that combination therapies require more thought and coordination. “Plastic surgery, in general, focuses on superficial organ systems such as skin, fat, and some occasional muscle work,” he explains. “These can be typically anesthetized with local numbing agents, such as lidocaine, but it can be challenging to keep people calm and control their pain for an extended period of time.” Even so, “with judicious use of medicine and a well-formulated plan, many things can be done under local,” he says.
To keep conscious or semi-conscious patients comfortable during cosmetic surgery, Dr. Unger creates a tranquil OR environment. “We put on soothing music and talk in calm, low, and consistent volume voices,” he shares. “It tends to make patients so relaxed they fall asleep during the procedure. It’s so calm.”
The Takeaway
While still experimental, the researchers at MD Anderson are optimistic about the potential hypnosis has to help patients recover faster (with less medication and fewer side effects). Plastic surgeons agree that the method could prove effective for patients who are amenable to the technique and better equipped to manage feelings of pain naturally.
More Related Articles
Related Procedures
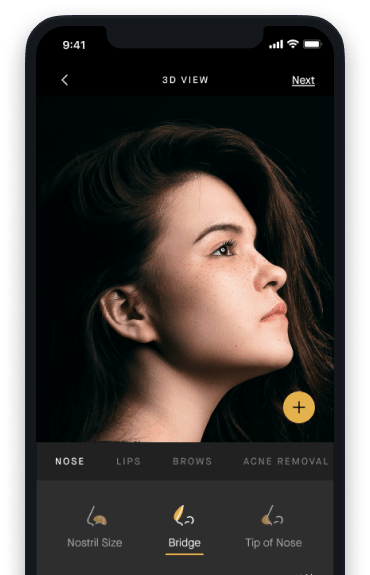
AI Plastic Surgeon™
powered by'Try on' aesthetic procedures and instantly visualize possible results with The AI Plastic Surgeon, our patented 3D aesthetic simulator.


