 Intralesional Steroid Injection
Intralesional Steroid InjectionEczema vs. Psoriasis: What’s The Difference?
To the untrained eye, it can be difficult to distinguish between the red, scaly patches of skin. Here’s what you need to know about the common skin conditions.
It’s believed that about 7.5 million Americans have psoriasis and another 32 million or so have eczema. That combined population is likely used to experiencing dry and scaly patches, which is why it can be easy for the untrained eye to misidentify the two. “Eczema, or atopic dermatitis, and psoriasis are both very common skin conditions that are often confused by non-dermatologists,” says Samer Jaber, MD, a board certified dermatologist and founder of Washington Square Dermatology in New York City. “They are both red, dry, scaly and often itchy, so they can look similar to non-dermatologists.”
To the trained eye, however, that’s where the similarities between eczema and psoriasis usually end. In order to give your skin the care it needs, a proper diagnosis from a board certified dermatologist is key. To give us non-dermatologists a better understanding of the ins and outs of eczema and psoriasis, we’ve tapped two top physicians for their expert insight.
Eczema & Psoriasis 101
Both eczema and psoriasis are skin conditions that, in some instances, present similarly. According to Marisa Garshick, MD, a NYC-based board certified dermatologist, they can appear as “red patches and plaques” on the skin, but “the causes, triggers, appearance, and treatment may differ between the two conditions.” In terms of similarities, eczema and psoriasis “are both conditions that reflect inflammation in the skin,” she shares – though “they occur for different reasons and can appear differently on the skin.” In terms of visible differences, Dr. Jaber says “psoriasis is typically more thick and scaly than eczema,” while eczema is often itchier than psoriasis.
With that in mind, let’s take a closer look at each:
What Is Eczema?
Also known as atopic dermatitis, eczema “describes a condition when the skin becomes red, itchy, dry, and, sometimes, flaky,” Dr. Garshick shares. It is often genetic in etiology (if your parents had eczema, you likely will, too), and it “commonly appears in babies or early childhood,” she adds. While Dr. Jaber says that it “can improve as you get older,” it is “often seen in patients that also have allergies and asthma.”
Eczema can affect any part of the body, but Dr. Jaber says it is more common “on areas that rub” such as “the inner elbow, behind your knees, neck, and arms, and legs.” Generally speaking, eczema is due to inflammation of the skin and is often triggered by irritants and things that dry out it out like harsh soaps, detergents, chemicals, clothing with a rough texture (think: wool), and stress. While we might think of cold winter climates as a culprit, warmer weather can exacerbate the condition, too. “For some people, intense heat and humidity can also aggravate the skin,” Dr. Garshick says. That includes hot showers.
Your Eczema Cheat Sheet
Causes & Triggers:
- Inflammation
- Genetics
- Environmental factors
- Stress
What it looks like:
- Dry, itchy areas of skin
- Patches of red, gray, brown, or purplish skin
- Affected areas can also be bumpy or uneven
Associated conditions:
- Seasonal allergies or hayfever
- Asthma
- Family history
Common treatments:
- Moisturizing, fragrance-free beauty routine
- Lifestyle changes (i.e. shorter showers, humidifiers, etc.)
- Biologic medications
No two eczema experiences are the same. In mild cases, there may be just a bit of redness or flaking. In more severe instances, the skin can thicken, be very red, and peel. At its worst, it can put the skin at risk for superficial infections. Treatment can range from over-the-counter skincare to prescription medication depending on the severity.
What Is Psoriasis?
Psoriasis is “an inflammatory skin condition that is characterized by red, scaly, well-demarcated plaques with silvery scales that can occur anywhere on the body,” Dr. Garshick explains. Unlike eczema, “psoriasis usually starts in adulthood and rarely occurs in children,” Dr. Jaber notes. Studies show there may be a hereditary component, and it can be associated with diabetes and heart disease. The average age of onset generally occurs at two different peaks. According to Dr. Garshick, the first is 15 to 35 years old and the second is 55 to 60 years old.
Common areas that are affected by psoriasis include the scalp, elbows, knees, lower back, nails, hands, and feet. “Psoriasis tends to affect the extensor surfaces, such as the knee and elbow, and can be associated with joint pains and psoriatic arthritis,” Dr. Garshick shares. Flare-ups can be brought on by a variety of factors. “Psoriasis is often triggered by changes in the season, stress, alcohol, and skin trauma,” Dr. Jaber says. It can also be exacerbated in the aftermath of infections like strep throat, he adds.
Your Psoriasis Cheat Sheet
Causes & Triggers:
- Injury (think: insect bites, sunburn)
- Certain illnesses & medications
- Temperature changes
- Smoking & alcohol consumption
What it looks like:
- Red or pink plaques
- Raised rash with scales
- Clearly defined patches
Associated conditions:
- Psoriatic arthritis
- Certain autoimmune conditions, including Crohn’s disease
- Type 2 diabetes
Common treatments:
- Topical steroids
- Vitamin D analogs
- Narrowband phototherapy
- Lifestyle changes (i.e. diet, stress, etc.)
Eczema and psoriasis are similar in that every case is different. The condition usually manifests in unpredictable cycles that alternate between periods of few to no symptoms and more intense flare-ups. For some, psoriasis is a mostly cosmetic concern. But, for others, it can cause discomfort (physical and mental) and impact quality of life.
Diagnosing Eczema & Psoriasis
If you are experiencing patches of scaly skin, the best way to determine whether you have eczema, psoriasis, or another skin condition is to schedule an appointment with your dermatologist. “In addition to the locations involved, associated symptoms, and the characteristic appearance, the most definitive way to distinguish the two is with a skin biopsy,” Dr. Garshick says. While the latter may be the most definitive, it’s not foolproof. “There are scenarios when even that is not conclusive to differentiate the two,” she admits.
When it comes to the physical exam, there are some specific indicators to keep an eye out for. “Eczema tends to be more ill-defined in the edges, while psoriasis is more well-demarcated,” Dr. Garshick explains. “Psoriasis is also known to experience the Koebner phenomenon, which is the appearance of new skin lesions in areas of skin trauma or injury in otherwise healthy appearing skin.”
Diagnosis may, however, be a little more nuanced on the face. Dr. Garshick says that it can sometimes be “challenging” to distinguish between eczema and psoriasis on the face – though “there are some hints based on location.” Because people with eczema tend to have more sensitive skin in general, it “tends to favor the area around the eyes and mouth” and can be “more pronounced in areas of the face where the skin is thinner,” Dr. Garshick shares. This is not usually true of psoriasis. “On the face and scalp, some individuals can experience an overlap of psoriasis and seborrheic dermatitis (dandruff), which can affect the hairline, forehead, and eyebrows,” she adds.
Treating Eczema & Psoriasis
Not only can a dermatologist diagnose your skin condition, but they can develop a treatment plan for it, too. “A dermatologist can help guide you on how to distinguish psoriasis from eczema as well as the specific treatment course,” Dr. Garshick says. This may include over-the-counter and prescription skincare, oral and injectable medications, and in-office procedures. “While the types of treatments may be similar – as both can be treated with topical creams as well as light therapy and oral or injectable medications – the specific ways and medications to treat the conditions can differ,” she notes. “It is always important to see a dermatologist to determine the best treatment options for you.”
How to Treat Eczema
There are many ways to treat atopic dermatitis, and many of them require little to no professional intervention. “I always recommend starting out with simple lifestyle changes,” Dr. Jaber says. These modifications include:
- Using a fragrance-free soap
- Taking shorter, cooler showers
- Patting (not rubbing) your skin dry
- Moisturizing twice a day
- Running a humidifier at home
- Avoiding fragrance & skin irritants
With your skincare routine, it’s all about preventing dry skin and irritation, but know that these changes may not be enough for everyone. “If, despite this, you still struggle with eczema, see a dermatologist for topical prescription medications,” Dr. Jaber says. “There are both steroid and non-steroid topical medications that work very well for mild to moderate eczema.” From a prescription perspective, Dr. Garshick points to non-steroid anti-inflammatory creams like Eucrisa® (crisaborole) and Elidel® (pimecrolimus) and injectable Dupixent® (dupilumab). For some patients, light therapy may also be effective. In the most severe cases, Dr. Jaber says there have been “some amazing advancements” in the treatment of eczema with biologic medications.
How to Treat Psoriasis
Psoriasis flare-ups can be unpredictable, and, as Dr. Garshick shares, “treatments do not provide a permanent cure” and “there’s always the chance it can come back.” Even so, there are some lifestyle adjustments that can help manage and maybe even prevent relapses. They include eating a well-balanced diet, maintaining a healthy body weight, keeping stress levels in check as much as possible, and many of the eczema-prevention tips outlined above. “Since psoriasis has been found to be associated with other medical conditions, such as an increased risk of heart disease, certain lifestyle modifications, such as weight loss and exercise, can be helpful for those with psoriasis and has been shown to improve psoriasis skin severity,” she notes.
From there, a multi-modal treatment plan often works best. Both of our experts agree that topical steroids and/or topical vitamin D analogs, like calcipotriene, can be effective – especially in the treatment of mild psoriasis. For moderate to severe cases, narrowband phototherapy and biologic medications are often a solution. As Dr. Garshick explains, the latter are “injections that target the immune system” and “have been a great advance” in the treatment of psoriasis because they allow patients to see results and clearer skin “relatively quickly.”
In terms of at-home skincare, Dr. Garshick says exfoliating acids can help to smooth scaly skin. “As some of the plaques can be thick, it can be helpful to use salicylic acid-based creams on the plaques to help exfoliate and eliminate the dead skin cells,” she shares. Oh, and then there is this piece of advice that is true of psoriasis and pretty much every other skin concern: Don’t touch it. “You don’t want to manually pick off the scales in psoriasis, as that can trigger more scales,” she warns.
The Takeaway
If you have red, rough patches of skin that are not responding to your usual hydrating skincare routine, it’s time to visit the experts to figure out the root cause. Even an article as comprehensive as this one cannot replace the expert eye of a board certified dermatologist when it comes to diagnosing and subsequently treating both eczema and psoriasis. Once you know what skin condition you are dealing with, you’ll be able to establish a treatment plan – including the necessary lifestyle adjustments – accordingly.
More Related Articles
Related Procedures
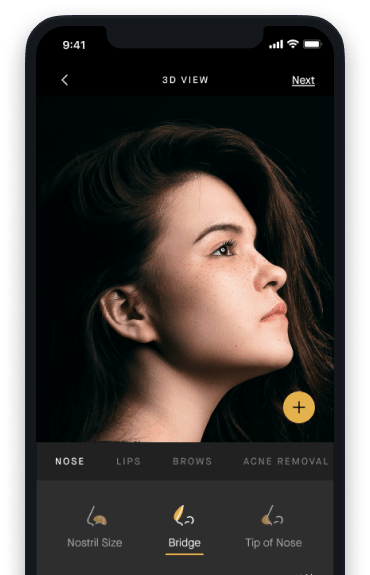
AI Plastic Surgeon™
powered by'Try on' aesthetic procedures and instantly visualize possible results with The AI Plastic Surgeon, our patented 3D aesthetic simulator.
