 Jawline Slimming with Botox
Jawline Slimming with BotoxWhy Botox For TMJ Disorders And Jaw Slimming Is On The Rise
While Botox® is FDA-approved to treat frown lines, forehead lines, and crow's feet, there are an array of 'off-label' uses as well. One such case gaining popularity? Using Botox® to treat temporomandibular joint disorder and, in turn, slim the jawline.
We all know that Botox® (onabotulinumtoxinA) can be used to smooth fine lines and wrinkles, but it can also do so much more. While the U.S. Food and Drug Administration (FDA) has approved the use of Botox® to temporarily improve the appearance of frown lines between the eyebrows, forehead lines, and crow's feet, there are an array of 'off-label' uses as well. One such case gaining popularity? Using Botox® to treat temporomandibular joint disorder (a.k.a. TMJD or TMD) and, in the process, slim the jawline.
What Is Temporomandibular Joint Disorder?
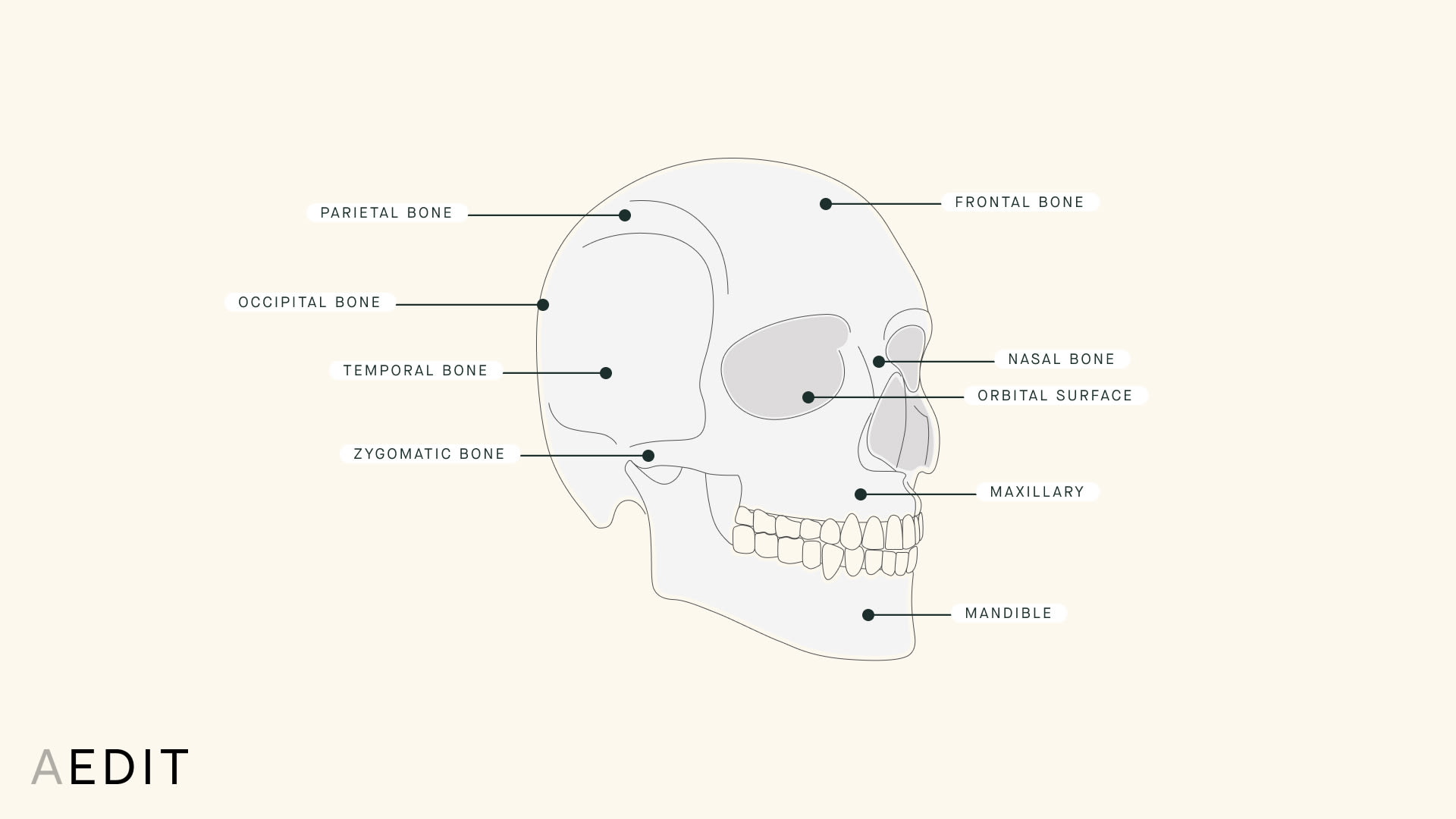
The temporomandibular joint (colloquially known as TMJ) connects the mandible (i.e. lower jaw) to the temporal bone (i.e. skull). It is present on both sides of the face and facilitates the opening and closing of the mouth, which, in turn, allows for speaking and eating.
The Anatomy of the Face & Jaw:
Temporomandibular joint disorder refers to a group of conditions that cause pain and discomfort around the jawline and neck. It can be triggered by a variety of things, including regular teeth grinding or jaw clenching (especially at night), arthritis, erosion of the joint, or structural problems. In addition to jaw pain, symptoms include jaw stiffness, tension headaches, limited jaw mobility, lockjaw, clicking or popping, and a change in teeth bite.
While there is no universal standard for diagnosing TMJD, the National Institute of Health (NIH) estimates that over 10 million people in America are affected by TMD and most of them are women. Board certified plastic surgeon Jonathan Cabin, MD, treats an increasing number of TMJD patients at his Beverly Hills practice and attributes the rise to three key factors:
- Increased Prevalence of TMJD: We live in a stressful world and a lot of people “express” this stress while subconscious and sleeping through jaw clenching and teeth grinding, which, in turn, has led to an increase in cases.
- Increased Recognition and Diagnosis of TMJD: For a long time, TMJD was an under-diagnosed condition mostly because the symptoms associated with it were mistaken for other disorders, like ear infections or migraine headaches. Now that providers can more properly diagnose TMJD, more people are aware they are suffering from it.
- Increased Awareness of Treatment Options: The internet and social media have led to a hyper-educated patient population who is now more likely to hear about TMJ treatment.
Dr. Cabin treats patients of all ages for TMD, but he reports that patients are diagnosed with the condition for different reasons at different ages. While most younger patients experience TMJD as a result of stress, older patients tend to have TMJD that is associated with dental issues.
How to Treat TMJ
- Over-the-Counter Pain Medication (think: ibuprofen)
- Bite Guards and Stabilization Splints to prevent clenching and grinding
- Ice packs to reduce swelling
- Stress Management
- Botox®
The NIH recommends over-the-counter pain medication or non-steroidal anti-inflammatory drugs (think: ibuprofen) to manage the pain associated with TMD. Additionally, bite guards and stabilization splints can be worn overnight to help provide relief for patients who are prone to clenching and grinding, and, in terms of day-to-day behavior, TMJD sufferers are generally encouraged to avoid hard foods and gum, apply cold packs to reduce swelling, stretch the mouth and jaw regularly, and practice stress management.
“When injected into the masseter muscles, Botox® reduces the strength of these muscles to the point where grinding and clenching can’t generate the same level of force, and thus, can’t generate the same level of damage,”
Jonathan Cabin, MD
Gaining popularity in the treatment and management of TMJD is the use of Botox® to relax the masseter facial muscle, which sits at the back of the mouth and plays a major role in chewing food and, yes, clenching and grinding teeth.
“The main muscle involved in the clenching and grinding force is the paired masseter muscle, which sits toward the back of the mouth on either side of the jaw. It can be seen bulging in and out of the lower face while chewing,” Dr. Cabin explains. “Believe it or not, these muscles are the strongest in the entire human body per unit weight, and this type of force likely evolved given our needs as hunter-gatherers to eat uncooked and, thus, unsoftened foods. But in our modern society, we only need a fraction of this strength to properly chew our food.”
Injecting a neurotoxin like Botox® into the masseter muscle can help counteract the force of the chewing, clenching, and grinding action that leads to damage and inflammation of both the teeth and jaw. “When injected into the masseter muscles, Botox® reduces the strength of these muscles to the point where grinding and clenching can’t generate the same level of force, and thus, can’t generate the same level of damage,” Dr. Cabin says. “With the right amount of Botox® injected with skill, the ability to chew normally — which requires a lot less force than our muscles are otherwise capable of — is not impacted at all.”
Is Botox® for TMJ Disorders Effective?
First things first, let’s talk about safety. It’s important to note that the injection of Botox® into the masseter muscles is off-label (read: not FDA approved). While it is widely considered by the medical community to be both safe and effective for short-term use, a 2017 study found that repeated Botox® injections into the masseter muscle decreased muscle thickness and bone volume in the mandibular gonial angle area (a.k.a. the jawline). Because findings about the long-term safety and efficacy of the treatment are inconsistent, the NIH provided a grant for further research about the risks and benefits of masseter Botox®.
One thing is clear: Patients have reported improvements in their TMJ pain after Botox® treatments. Like most Botox® injections, this procedure is quick and requires minimal downtime. Typically, TMJD treatment includes four injections on each side of the jaw muscle, for a total of eight injections. Although the injections are deeper than other cosmetic uses, the process is relatively painless. Dr. Cabin recommends using the smallest needles possible in combination with a vibrational device against the skin to minimize discomfort.
“After carefully reviewing the procedure and any potential side effects, I have my patients use an ice roller over the intended injection areas for a few minutes to help to reduce discomfort and any chance of bruising,” he explains. “I then ask my patients to clench down, which activates the masseter muscles and allows me to outline them carefully with a skin pencil. This is for precision and to ensure symmetry between the two sides.”
The most common side effect following masseter Botox® is discomfort in the muscle — particularly when activating the muscle while chewing food or talking — for the first 24 hours after treatment. Dr. Cabins explains just like a vaccination in the arm muscle can leave the area feeling achy for the first day or so, an injection into the masseter muscle is no different.
Depending on the strength of the masseter muscle and the amount of neurotoxin required, some patients may experience temporary changes in their ability to chew. “Patients with particularly strong and/or large muscles may require a greater amount of Botox®. In these patients, there is sometimes a transient reduction in the ability to chew tough foods, like steak, which generally lasts only a few weeks,” Dr. Cabin says. “Rarely, a patient with normal amounts of Botox® will report this side effect, as well.”
How Long Does Botox® for TMJD Last?
- Downtime: 24 hours of injection site and/or muscle pain
- Initial Results: Within 2 weeks
- Peak Results: Within 4 to 6 weeks
- Lasts: 3 to 5 months
Like all Botox® injections, the results of TMJD treatment are not immediate. For masseter injections, it typically takes a minimum of two weeks to see changes to both pain levels and jaw shape. Dr. Cabin says that relief usually increases over the course of the first month and peaks at about four to six weeks post-treatment. At the same time, patients will also notice a cosmetic difference in their face and experience jaw narrowing and slimming.
Depending on the patient, results can last anywhere from three to five months. As the Botox® begins to wear off and the masseter muscle expands, patients will notice a reversal in facial structure and TMJD symptoms. To sustain a slimmer jawline and keep TMD discomfort to a minimum, patients can schedule additional treatment before the Botox® fully wears off. Once a patient has a good sense of how long it lasts for them, they can go in for routine re-injections.
The Takeaway
While the long term ramifications of Botox® injections into the masseter muscles remains inconclusive, its effectiveness as a treatment for TMJD and jaw slimming is not. Just a few injections of the neurotoxin into the masseter muscle can help to relieve TMD symptoms and refine the size and shape of the jaw. The quick and (relatively) painless procedure lasts up to six months and costs anywhere from $450 to $1,500, depending on the practitioner. And, as with any procedure, be sure to find a board certified plastic surgeon or dermatologist who specializes in the technique.
More Related Articles
Related Procedures
AI Plastic Surgeon™
powered by'Try on' aesthetic procedures and instantly visualize possible results with The AI Plastic Surgeon, our patented 3D aesthetic simulator.
